Any professional in the Pharma and Clinical Research Industry should be aware of what GCP stands for, as it has now become an integral part of the business model of all big organisations in this sector. Good Clinical Practice (GCP) is internationally recognized set of ethical and scientific standards, provided by ICH, for the design, conduct, performance, monitoring, auditing, recording, analysis, and reporting of clinical trials or studies. Its purpose is to protect the rights, safety and welfare of people who participate in researches and to deliver informative, reliable and credible data. GCP can actually be applied for different aspects of any given company, such as:
– GCP for Cosmetics
– GCP for Investigators
– GCP For Monitors
– GCP for Medical Devices
– Veterinary GCP
And others.
But why is GCP so important? In order to properly and fully comprehend its significance, we have to go back to the roots of ICH-GCP and look at its historical background and inception. What led to the creation of GCP guidelines in the United States and Europe and also to the genesis of the ICH is a series of events which occurred in the past. Those events were linked to a range of clinical trials that happened to be unsuccessful and resulted in ineffectiveness. The first indicator in the regulation of drugs is the Food and Drugs Act established in the United States far back in 1906. It is considered to be the result of deadly and very dangerous drugs that could have been sold legally just like any other consumer product. For instance, such drugs were ‘Grandma’s Secret’ and ‘Kopp’s Baby’s Friend’. They contained a huge amount of morphine. ‘Dr King’s Consumption Cure’ and ‘Dr Bull’s Cough Syrup‘ are examples of drugs which had large doses of morphine and chloroform too.
After the Food and Drug Administration (FDA) approved the Federal Food, Drug and Cosmetic Act in 1938, manufacturers were required for the very first time to not only test drugs for safety but also show evidence that guarantees the safety and efficiency of the product. Later on in 1982, the World Health Organization (WHO) along with the Council for International Organizations of Medical Sciences (CIOMS) presented the ‘International Guidelines for Biomedical Research Involving Human Subjects‘ which served to help progressing countries obtain the principles of the Declaration of Helsinki and the Nuremberg Code.
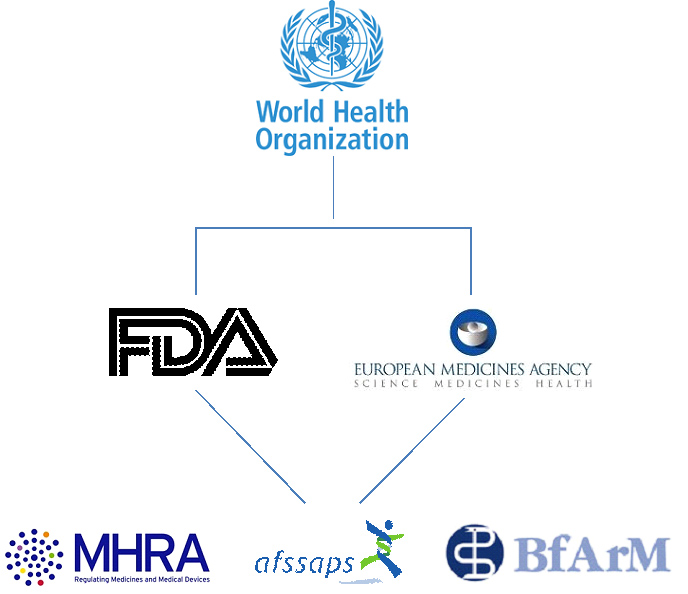
Nevertheless, there is a diverse range of appointed regulations for each country set by the organization which stays on top of the hierarchy. This is the World Health Organisation (WHO), followed by European Medicines Agency (EMA) and Food and Drug Administration (FDA) in Europe and the USA respectively. Still, most countries have their local authorities such as MHRA in England and Bfarm in Germany. This pyramidal-like structure still keeps different standards real.
Why? Because even though they share the same concepts, some of them demand different focus and requirements. So, in spite of the Informed Consent Form being a standard document anywhere in the world, when it concerns GCP, some significant differences are likely to be found in it. Such differences depend on the type of the trial, the country in which the trail is performed and the regulatory authority that is in charge of Good Clinical Practice.
The world of clinical research is developing at a high speed. So the question that arises is whether or not ICH-GCP guidelines should be changed in order to become more reasonable, more effective and more present-day-oriented. Are the current guidelines too broad and general? Or are they specific and informative enough? Should it be standardized or should they develop new sets of guidelines for each different GCP, like the Veterinary GCP? What do you think?